Active Proteins
Active Proteins Full Catalog
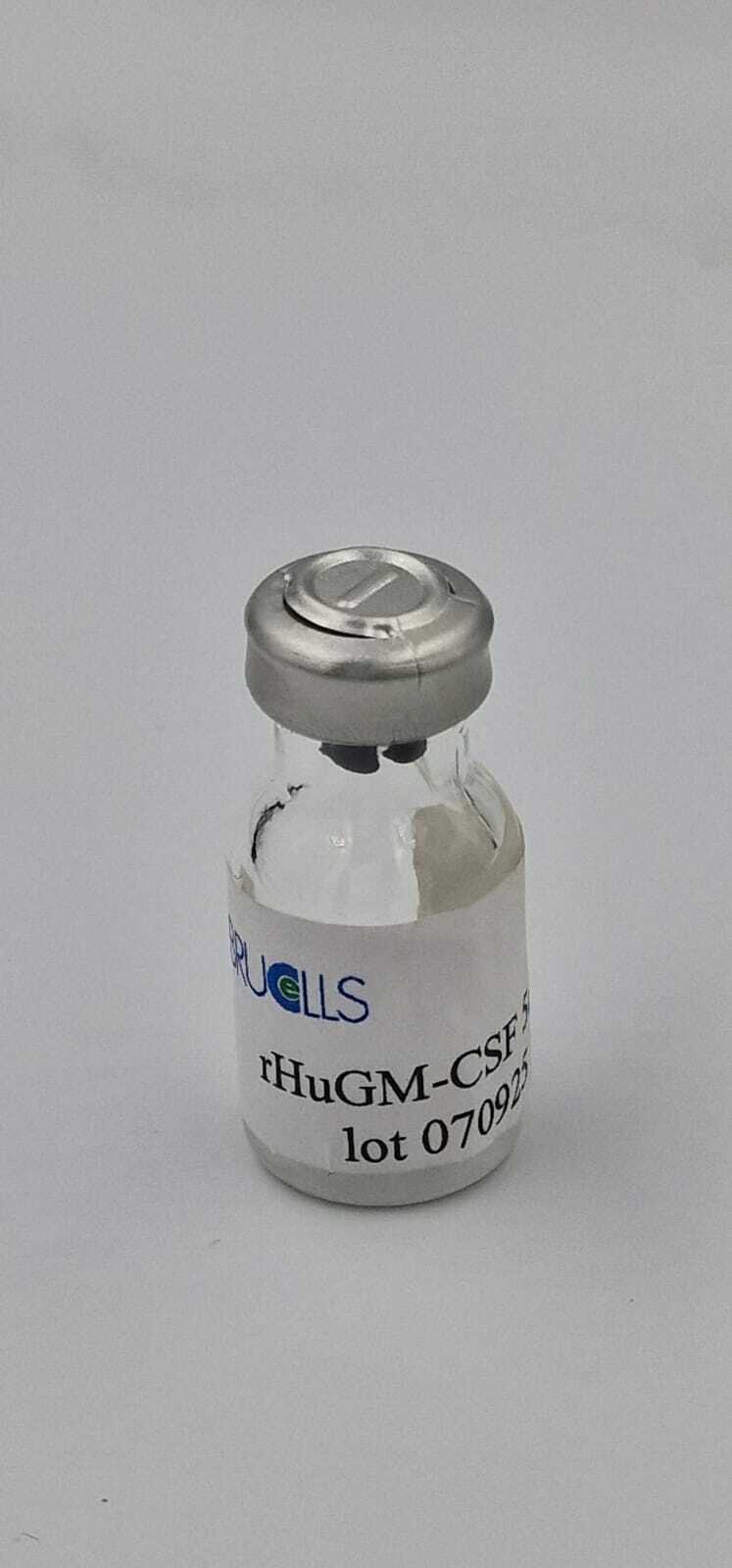
Cusabio's active proteins available from Gentaur:
-
- Cusabio produces recombinant proteins using advanced technologies, ensuring high purity and biological activity. These proteins are cytokines, growth factors, enzymes, signaling molecules and antibodies.
-
Bioactive Proteins:
- Proteins offered by Cusabio are bioactive, meaning they retain their native structure and function. This is essential for cell culture with endogenous proteins in biological systems.
-
Application-Specific Proteins:
- Cusabio's active proteins are tailored for specific applications, such as cell culture experiments, in vitro assays, or other research applications including tagged proteins.
-
Custom Protein Production:
- Cusabio provides custom protein production services throug Gentaur, allowing researchers to request specific proteins tailored to their experimental needs.
-
Quality Control:
- Cusabio uses quality control measures to ensure the purity, activity, and consistency of the active proteins. This includes SDS-PAGE, HPLC, and functional assays.
-
Range of Targets:
- Active proteins may cover a broad range of biological targets, including growth factors, cytokines, chemokines, enzymes, hormones, and signaling molecules.